THE SMARTEST CUTS FOR HEALTH
The Star
August 31, 2025
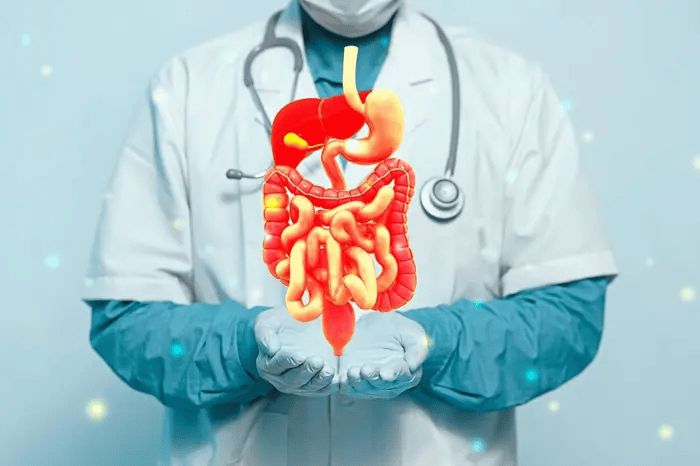
Upper GI disorders and obesity-related digestive conditions are very common, and often, many Malaysians suffer in silence due to lack of awareness or even fear of treatment.
DO you often say you have “gastric”? Think it’s just part of stress and nothing serious?
As long as it goes away with some over-the-counter meds, you assume it’s fine, right?
If this describes you, then you need to seriously reconsider what’s normal, and seek help, sooner rather than later.
Upper gastrointestinal (GI) disorders and obesity-related digestive conditions are very common, and often, many Malaysians suffer in silence due to lack of awareness, or even fear of treatment.
However, advancements in medical technology and surgical techniques are significantly changing the way these conditions are managed.
From minimally-invasive techniques to robotic-assisted surgery, cutting-edge GI procedures are now offering patients safer, faster and more effective outcomes than ever before.
Hospital Picaso consultant gastroenterologist and physician Dr Chen Harn Chin notes that GI conditions account for a large number of medical consultations, both in general practice and specialist clinics.
“Among the most commonly treated conditions are gastroesophageal reflux disease (GERD), peptic ulcers, gallstones and gastric cancers,” he observes.
Consultant general and upper GI surgeon Dr Yeap Chee Loong adds that besides the conditions Dr Chen mentioned, consultations for obesity-related disorders are also quite common in his practice at Hospital Picaso.
“Obesity is a growing health crisis in Malaysia and can contribute to, or complicate, these GI conditions, increasing the risk of chronic acid reflux, fatty liver disease, and cancers such as stomach, oesophagus and colon cancers.
“Many patients do not realise that obesity significantly impacts overall and GI health,” he says.
“It could worsen conditions like GERD, and increase the risk of serious illnesses such as gastric cancer.”
Why early detection matters
The key to treating upper GI and obesity-related issues effectively lies in early detection.
Unfortunately, symptoms like heartburn, bloating, abdominal pain or unexplained weight changes are often ignored or self-medicated, delaying proper diagnosis.

According to Dr Yeap, cutting-edge surgery uses the latest methods and most advanced technology to improve surgical outcomes.
“Early symptoms can be subtle, and people tend to dismiss them until the condition has worsened,” notes Dr Yeap.
“By then, treatment becomes more complex, especially if the disease has progressed to an advanced stage or causes secondary complications.”
“If the patient has difficulty swallowing, or pain when swallowing; is passing out black stools or even vomiting blood; and has unexplained weight loss, such symptoms are what we call ‘alarm’ symptoms, and should be looked at immediately,” advises Dr Chen.
Dr Yeap adds: “In Malaysia, you often know or hear of people suffering from ‘gastric’ and they often dismiss it as part of their ‘stress’ from work and what not.
“If such symptoms are an early harbinger of GI cancer, and these symptoms are ignored and not investigated, the disease will progress.
“In Malaysia, most cases of upper GI cancers are diagnosed as advanced cancers (stages 3 and 4), making treatment very challenging.
“If the cancer was detected earlier, treatment would be much more effective.”
Dr Chen advises that we should seek medical advice even if the symptoms appear very general and non-specific, even “gastric”-like.
“In addition, the ‘alarm’ symptoms should immediately be looked at.
“And if you are above 40 years of age with new onset ‘gastric’ symptoms, you should be investigated as early as possible to rule out serious problems,” he says.
“In the development of cancer, you have a pre-cancerous stage.
“For example, if you have GERD, you can develop Barrett’s oesophagus (abnormal changes in the cells that line the lower oesophagus). [It] increases the risk of oesophageal cancer.
“Hence, if you are able to detect Barrett’s oesophagus first, you can actually treat it before it becomes full-blown cancer,” he explains.
Cutting-edge GI management and surgery
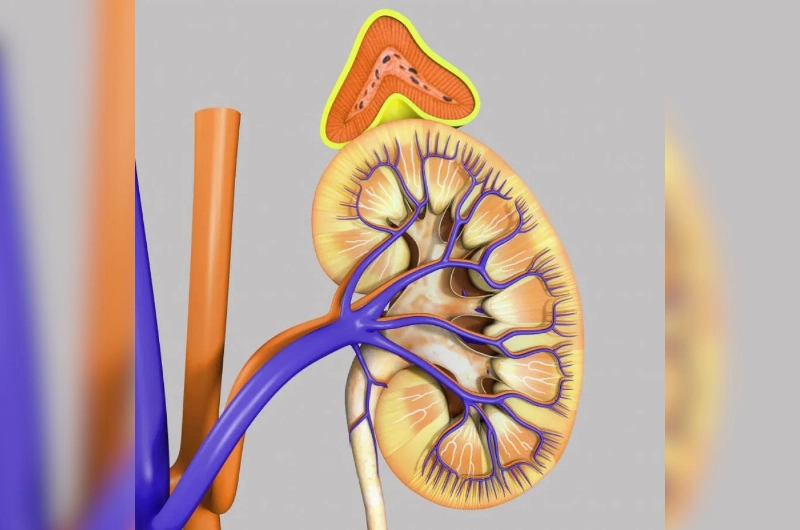
Modern diagnostic tools such as endoscopic imaging, high-resolution scans and functional studies now make it easier to detect GI disorders early.

Dr Chen notes that innovations in GI management and surgery is something that is progressively ongoing.
With improved accuracy and accessibility, patients can receive timely treatment and prevent complications, observes Dr Chen.
“Advancements in both surgical, as well as non-surgical, techniques have also significantly improved treatment outcomes.
“For instance, endoscopy today has advanced to the point that many surgeries can now be carried out endoscopically,” he adds.
The tools available to doctors today are also enabling them to perform minimally-invasive surgeries more often.
But today, cutting-edge techniques such as laparoscopic (keyhole) surgery and robot-assisted procedures are rewriting the rules.
“Cutting-edge surgery means we are using the latest methods and most advanced technology to improve surgical outcomes,” says Dr Yeap.
“These minimally-invasive techniques allow us to operate through small incisions with greater precision and control.
“This leads to less pain, reduced risk of infection and quicker recovery for the patient.”
In upper GI disorders, advanced surgery is used to treat many problems that previously could not be handled this way.
“The advances in robotic surgery has enabled us to treat more types of disorders with improved outcomes, even in cancer surgery.
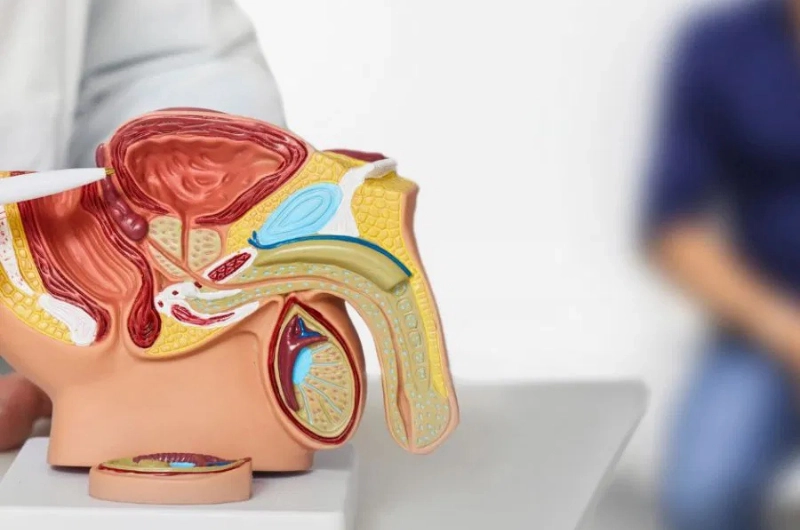
“And for patients with obesity, bariatric surgeries like sleeve gastrectomy, gastric bypass and duodenal switch are helping to improve not just weight loss, but also metabolic health.
“Many of these surgeries are now being performed laparoscopically or are robot-assisted,” he adds.
With advances in surgical techniques, bariatric surgery, once considered a last resort, is now recognised as a highly effective treatment for individuals with severe obesity or obesity-related complications, and it has become a more common procedure.
“It’s not just about weight loss – it’s about improving quality of life and reducing the risk of long-term diseases,” Dr Yeap notes.
“Patients often see improvement, remission or resolution for conditions such as type 2 diabetes, high blood pressure and sleep apnoea within months after surgery.
“This is why we also call it ‘metabolic surgery’ because it goes beyond weight loss to tackle underlying metabolic issues.”
“A newer innovation now is endoscopic sleeve gastroplasty.
“It’s quite similar to a sleeve gastrectomy, except that it’s done endoscopically.
“It’s another option for patients depending on their condition and preferences,” he adds.
However, there are strict criteria that need to be fulfilled before bariatric surgery can be performed.
These criteria involve the extent of patient obesity, as well as the presence of co-morbidities such as diabetes and so on.
Recovery and patient safety
Despite the high-tech nature of these surgeries, safety remains a top priority, says Dr Yeap.
While all surgeries carry some risk, the complication rates for advanced GI procedures are now lower than ever, thanks to better pre-operative screening, real-time monitoring during surgery and improved post-op care.
Successful GI and bariatric surgery is rarely the work of a surgeon alone.
“Today, patient care is a team effort involving various specialities and support staff. We look at the patient as a whole, not just the illness,” emphasises Dr Chen.
“A patient undergoing bariatric surgery, for example, also needs nutritional guidance, emotional support and long-term lifestyle counselling to maintain results.
“A patient undergoing GI cancer treatment needs a multidisciplinary team for management.
“This team often includes the gastroenterologist, surgeon, pathologist, radiologist, oncologist and so on,” he says.
This holistic model ensures that patients not only recover from surgery but also adapt to new habits that support lifelong health and wellness, emphasises Dr Yeap.
“It’s not only doctors, but also the support staff who help with the patient’s journey to wellness. Teamwork is vital.”
Innovations in GI management and surgery is something that is ongoing progressively, notes Dr Chen.
“Robotic platforms are becoming more refined, offering even greater precision. Artificial intelligence (AI) is being incorporated into diagnostic endoscopy and surgical planning.”
As these innovations become more widely adopted, the hope is that more patients will benefit from early, effective intervention – improving not just survival, but also long-term quality of life.
Dr Yeap opines that such advances, especially in AI innovations, will not replace the “human touch” in patient counselling and treatment.
“However, it will replace doctors who do not embrace or adopt such technology.”
Don’t wait – get checked
Despite these advancements in GI care, many Malaysians remain unaware of the options available to them – or they delay seeking help due to ignorance, misconceptions or fear.
Some worry that surgery is too risky, while others believe it is only for extreme cases.
If you’re struggling with persistent digestive issues, severe acid reflux, unexplained weight changes or obesity-related symptoms, don’t wait until it’s too late.
Modern GI surgery offers options that are safer and more effective than ever before.
Talk to your doctor, get screen-ed if needed, and explore the possibilities of cutting-edge GI care – it could be the start of a new chapter in your health journey.
Hospital Picaso is committed to delivering high-quality care through the latest advanced surgery and integrated oncology services with experienced upper GI specialists. To learn more, visit www.hospitalpicaso.com.
KKLIU 2701 / EXP Dec 31, 2027
Source
THE SMARTEST CUTS FOR HEALTH (The Star, 31 August 2025)
Reference