Cancer Care 101: Understanding Symptoms, Treatment Options and Life After Diagnosis
February 13, 2026

A cancer diagnosis often arrives without warning and can feel deeply unsettling, not only for patients, but also for those closest to them. In the days that follow, many questions surface naturally: What does this diagnosis really mean? What treatments are available? How will life change from here?
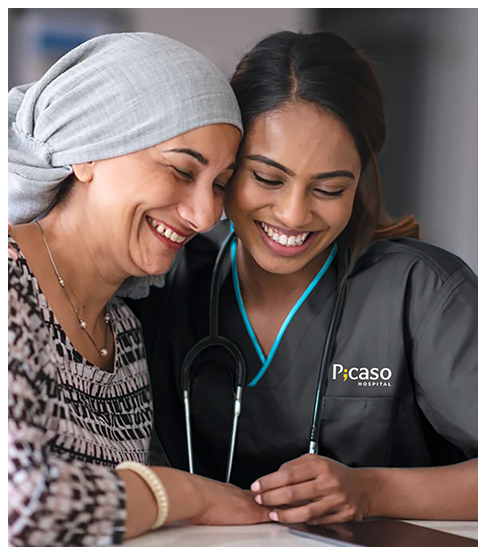
As oncologists involved in both cancer treatment and supportive care, our cancer centre team at Hospital Picaso in PJ, Malaysia, we see firsthand how important clarity and reassurance are at this stage. Cancer care today has evolved significantly. It is no longer focused solely on treating disease, but on providing personalised, coordinated care that supports physical health, emotional well-being, and quality of life throughout the journey.
At our Cancer Centre in Petaling Jaya, cancer care is delivered through a multidisciplinary approach that reflects both international standards and the needs of patients.
Noticing the Early Signs and Knowing When to Seek Medical Advice
Cancer can present in many different ways, depending on its type, location, and stage. Some symptoms may appear subtle at first and are often mistaken for common health concerns. While most symptoms are not caused by cancer, changes that persist or worsen over time should be medically assessed.
Symptoms that warrant evaluation include:
A lump or swelling that does not reduce or resolve
Unexplained weight loss or persistent loss of appetite
Ongoing pain, unusual fatigue, or shortness of breath
Changes in bowel habits or urinary patterns
Unusual bleeding or discharge
A chronic cough, hoarseness, or difficulty swallowing
Wounds or skin changes that do not heal
In Malaysia, where cancer is often diagnosed at a later stage, early detection remains one of the most important factors in improving outcomes. When symptoms last more than a few weeks, interfere with daily activities, or continue to progress, seeking medical advice early allows timely investigations and appropriate referral.
Making Sense of a Cancer Diagnosis and What Comes Next
Hearing the word “cancer” can be frightening, but it is important to understand that a diagnosis today is not a single, fixed verdict. Rather, it marks the beginning of a structured and carefully planned process.
A cancer diagnosis typically includes:
The specific type and location of cancer
The stage of disease, indicating how far it has spread
Tumour characteristics, such as hormone receptors or genetic markers
The patient's overall health, lifestyle, and personal circumstances
These details guide doctors in developing a treatment plan tailored to each individual. Cancer care is no longer “one-size-fits-all.” Instead, treatment decisions are increasingly personalised, balancing medical evidence with the patient’s goals, preferences, family considerations, and daily realities.
Open and honest communication remains essential. Patients are encouraged to ask questions, clarify uncertainties, and take an active role in decisions about their care.
Understanding Your Treatment Options and How Decisions Are Made
Most patients receive care from a multidisciplinary team that brings together expertise from different specialties to ensure comprehensive and coordinated treatment. Our multidisciplinary cancer centre team includes oncologists, surgeons, radiologists, pathologist, palliative care physicians, nurses, dietitians, rehabilitation professionals and counsellors.
Treatment options at our cancer centre may include:
Surgery remains an important treatment option for many cancers, particularly when the disease is localised. Today, surgical care has advanced significantly beyond traditional open surgery. Depending on the cancer type and location, patients may be suitable for minimally invasive approaches, such as laparoscopic or robotic-assisted surgery, which aim to reduce surgical trauma, shorten recovery time, and preserve function.
In selected cases, non-surgical or image-guided techniques may also be considered, especially for patients who are not ideal surgical candidates. The choice of approach is carefully assessed to balance effectiveness, safety, and recovery.
Chemotherapy uses anti-cancer medications to destroy cancer cells or slow their growth. It may be given before surgery to shrink a tumour, after surgery to reduce the risk of recurrence, or as a primary treatment when surgery is not appropriate. Treatment plans are tailored to minimise side effects while maintaining effectiveness.
Radiotherapy delivers precise, high-energy radiation to cancer cells while limiting exposure to surrounding healthy tissues. It may be used alone or in combination with surgery and chemotherapy, depending on the clinical situation.
These newer treatments represent significant advances in cancer care. Targeted therapies work on specific molecular pathways involved in cancer growth, while immunotherapy helps the body's immune system recognise and attack cancer cells. These options are offered to selected patients based on tumour biology and individual suitability.
For hormone-sensitive cancers, such as certain breast and gynaecological cancers, hormonal therapy may play a central role. These treatments work by blocking or reducing the effects of hormones that drive cancer growth and are often used as long-term therapy to reduce the risk of recurrence.
In some patients, genetic testing may be recommended to assess inherited cancer risk or guide treatment decisions. Genetic counselling helps patients and families understand the implications of test results, including screening recommendations and preventive strategies for relatives.
Palliative care plays an important role at any stage of cancer, not only in advanced illness. It focuses on:
Relieving pain and physical symptoms
Managing treatment-related side effects
Supporting emotional and psychological well-being
Enhancing overall quality of life
The most appropriate treatment plan considers medical effectiveness, potential side effects, personal values, cultural context, and long-term goals, ensuring care remains aligned with what matters most to the patient.
What Is Palliative Care and Why It Matters
“Palliative care is not about giving up treatment. It is about making sure patients are comfortable, supported, and heard at every stage of their cancer journey.”
Palliative care is often misunderstood as care reserved for the final stages of illness. In reality, it can be introduced early and provided alongside active cancer treatment to support patients throughout their journey.
This approach focuses on managing symptoms such as pain, fatigue, nausea, breathlessness, anxiety, and sleep difficulties, while also addressing the emotional and psychological impact of cancer. Importantly, palliative care works in partnership with oncology care, complementing treatments such as chemotherapy or radiotherapy rather than replacing them.
Support also extends to families and caregivers, helping them understand what to expect, navigate complex decisions, and cope with the demands of caregiving. At its core, palliative care is about preserving dignity, autonomy, and quality of life, regardless of the stage of illness.

Living Well During and After Cancer Treatment
Cancer care continues beyond the completion of treatment. Recovery, survivorship, and long-term well-being are integral parts of the journey.
Patients can support their recovery by:
Maintaining balanced nutrition and adequate hydration
Staying physically active within their abilities
Paying attention to emotional health, stress levels, and sleep
Attending regular follow-up appointments
Reporting new or persistent symptoms promptly
For some patients, survivorship care focuses on monitoring for recurrence and managing long-term treatment effects. For others, ongoing symptom control and supportive care remain important. Both approaches are valid and centred on individual needs and circumstances.
A Compassionate and Personalised Approach to Cancer Care
Advances in medical treatment, combined with personalised care planning and integrated supportive services, have transformed how patients experience cancer today.
With early medical attention, clear communication, and a compassionate multidisciplinary team, patients and families can feel supported at every stage.
No one needs to face this journey alone, and meaningful care extends well beyond treatment itself.
返回